Achieving Diversity in Clinical Trials
Diversity, equity, and inclusion (DE&I) are three closely linked values working together to support various groups of individuals, including those of different races, ethnicities, religions, abilities, genders, and sexual orientations.

What Does DE&I Mean for Clinical Research?
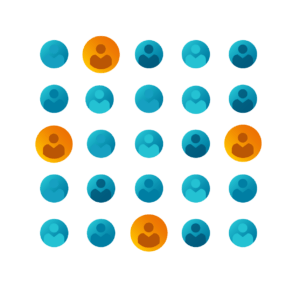
In order to effectively achieve DE&I in clinical research, there must be equal representation of underrepresented persons in clinical trials. Per guidance from the Food and Drug Administration (FDA), this includes representation in terms of gender equality, race and ethnicity, LGBTQ+, socioeconomic status, and more.
Studies have proven not all drugs or devices work effectively in every person, so it’s important to have diverse and equal representation in clinical trials to generate useful, inclusive data for regulatory review. Researchers must be able demonstrate they’ve cast the widest net possible in studying how people from a variety of different communities and backgrounds could each be affected by the investigational drug or device. Historically, marginalized communities have been underrepresented in clinical trials, resulting in incomplete data and potential harm from ineffective or dangerous treatments.
Achieving DE&I in clinical trials requires a concerted effort from clinical trial sponsors, researchers, healthcare providers, community organizations, and individual participants. By prioritizing diversity, equity, and inclusion, we can ensure clinical trials generate useful, inclusive data for regulatory review and develop safe and effective treatments that work for everyone.
Common Roadblocks to Diverse Clinical Trial Enrollment
Mistrust
 Mistrust of Clinical Trial Participation
Mistrust of Clinical Trial Participation
In 2020, the COVID-19 pandemic helped cast clinical trials in a new light, with more people understanding the important role they play in improving health. Until a few years ago, some individuals in the U.S. only heard about clinical trials via the news – and what they heard did not always inspire trust, with media coverage often focusing on clinical trial mishaps and other negative aspects.
To overcome mistrust in clinical trials, the industry must do more. Increased educational efforts are necessary to help the general population understand what happens in trials, why they matter, and the safety controls inherent to the research process. The more education there is about clinical trials, the better people generally perceive trials. An informed population is one that understands why clinical trials are important and isn’t fearful or hesitant of participating in clinical trials.
Education and outreach help potential participants understand that clinical trials are safe and effective, and the institutional review board (IRB) is in place to ensure participant protection at all times.
Engaging with communities and building relationships gives researchers an opportunity to have conversations and learn about unique community characteristics and needs.
History
 Historical Context and Abuses
Historical Context and Abuses
Some communities may mistrust clinical trials and be hesitant about contributing personal data due to historical mistreatment by medical professionals and the research community. Abuses like the Tuskegee Syphilis Study and the mishandling of Havasupai Tribe genetic information (to name just a few) have had a significant negative impact on the way underrepresented populations view research. And the pain of such exploitation is not easily forgotten, even across generations.
Overcoming such mistrust takes time and commitment to communication. It’s all about building trust. Working with boots-on-the-ground community members and leaders, and going to non-traditional locations such as community centers, community health organizations, and places of worship are key.
Community
 Community Engagement Strategies
Community Engagement Strategies
One way to build trust is by communicating the importance of volunteer participation in clinical trials. Providing transparency throughout the process, including trial design, development of desired endpoints, and the results of the trial, is another engagement tactic that can go a long way in building trust amongst participants. Seeking input into the elements of trial design that might impact community members’ ability to participate may also encourage participation.
One of the best ways to gain participation is to hear stories firsthand from current and former participants about their trial experiences. This can help potential participants understand what their experiences may be similar to – helping them to better picture themselves in the study and can encourage them to enroll into a trial.
Engaging with study staff and investigators of similar backgrounds can also be helpful for building trust among potential minority study participants. Seeing someone who “looks like me” or who is from a similar shared background can help make the clinical trial setting feel more familiar and comfortable to someone unsure about participating.
Environment
 Environmental Barriers
Environmental Barriers
Creating a network of clinical trial sites or research sites in underserved communities where potential participants already receive care can greatly improve clinical trial diversity. This is key to helping ensure clinical trials better reflect all patient populations.
Oftentimes, brick-and-mortar research sites are located in bigger cities; for some participants, this may mean driving hours one way for a visit. If sites are too far away, this may discourage people from volunteering their time altogether. Limited transportation access, competing work and family commitments, and other factors can compound the issue. Decentralized clinical trial modalities may be one way to make clinical trials more accessible.
Key Guidance and Regulation for DE&I in Research
FDA’s Draft Guidance
Provides sponsors with recommendations on how to develop a “Race and Ethnicity Diversity Plan” for new drug and device applications. This is a roadmap as to how Sponsors/CROs/sites will enroll diverse members from underrepresented racial and ethnic populations within the U.S.
Belmont Report
Written by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, the report identifies the basic ethical principles when conducting biomedical and behavioral research involving human subjects. The Report also discusses developing guidelines to assure research is conducted in accordance with those principles.
Declaration of Helsinki
Ethical principles surrounding medical research involving human subjects, developed based on past clinical trial atrocities.
21 CFR 56.111 and 45 CFR 46.111
Criteria for IRB approval of research includes assessing equitable selection of participants. “In making this assessment the IRB should take into account the purposes of the research and the setting in which the research will be conducted.”
21 CFR 56.11
45 CFR 46.111
21 CFR 56.107 and 45 CFR 46.107
Regulations describe the need for diverse IRB membership “including consideration of race, gender, cultural backgrounds, and sensitivity to such issues as community attitudes.” If the IRB regularly reviews research involving vulnerable populations, the IRB should include in its review one or more people knowledgeable about and experienced in working with such populations.
21 CFR 56.107
45 CFR 46.107
21 CFR 50 Subpart B and 45 CFR 46.116
Based on “respect for persons” from the Belmont report, this regulation outlines general requirements for informed consent, including basic and additional elements of that should be included in an informed consent document. Also advises against exculpatory language and requires minimized possibility of coercion and undue influence. Provides instruction on providing consent materials in a language understandable to the participant.
21 CFR 50 Subpart B
45 CFR 46.116
Featured Resources
Sickle Cell Disease: The Importance of Amplifying Patient Voices
Sickle cell disease significantly impacts the African American population, a minority community historically underserved by clinical research.
DEI in Clinical Research
We discuss the current state of DE&I in research, how tech can drive inclusivity, and the role of sites in engaging diverse participants.
Racial Diversity in Clinical Trials: Building Trust in Participant Engagement
COVID-19 has focused the importance of diversity, equity, and inclusion considerations in clinical trial enrollment. How can the research community address the root causes for lack of diversity? What actions ...



 Mistrust of Clinical Trial Participation
Mistrust of Clinical Trial Participation Historical Context and Abuses
Historical Context and Abuses Community Engagement Strategies
Community Engagement Strategies Environmental Barriers
Environmental Barriers